An Overview of Pulmonary Drug Delivery
Pulmonary drug delivery offers direct treatment to the lungs, bypassing the upper airways and mucociliary clearance. This route enables quick systemic absorption and distribution of drugs throughout the body. Inhalation products have seen significant advancements in recent years, particularly with small molecule formulations. The focus on particle size, deposition mechanisms, and flow rate ensures better delivery to target areas in the lungs. These improvements have helped treat conditions like cystic fibrosis and bacterial infections more effectively by targeting the site of action directly.
Small Molecules
Small molecules have become a cornerstone in pulmonary drug delivery. Their formulations are now optimized for particle size, flow rate, and deposition efficiency. The aim is to deliver the drug directly to the target areas in the respiratory tract for maximum therapeutic impact. This approach enhances treatment outcomes in diseases like cystic fibrosis and bacterial infections.
Effective delivery of small molecules through inhalation means better absorption and fewer side effects. Drugs can target the pulmonary epithelium directly, ensuring more localized effects and less systemic exposure. This localized targeting improves patient compliance and therapeutic outcomes.
Peptides and Proteins
Peptides and proteins offer significant therapeutic potential in treating respiratory diseases. Delivering these molecules through inhalation requires precise formulation design, focusing on particle size and deposition efficiency. Advances in formulation design now allow for more effective delivery of peptides and proteins directly to the lungs.
By using dry powder inhalers, peptides and proteins can reach the pulmonary epithelium directly, resulting in better absorption and therapeutic outcomes. This targeted approach minimises systemic exposure, which is beneficial for conditions like severe respiratory diseases and even some neurological disorders. Understanding the unique challenges of delivering peptides and proteins to the lungs ensures more effective treatments and better patient outcomes.
Vaccines
Pulmonary delivery is gaining traction in vaccine administration. Delivering vaccines through inhalation offers direct interaction with the respiratory epithelium, potentially boosting immune responses. This method has been applied in cases like inhaled insulin for diabetes and inhaled loxapine for psychiatric disorders.
One key benefit of pulmonary vaccine delivery is the fast absorption facilitated by the lungs’ rich blood supply. Dry powder inhalers and nebulizers allow for fine particles to deposit directly in the airways, optimizing the interaction with immune receptors on respiratory epithelial cells. This targeted delivery approach can improve vaccine efficacy, especially for respiratory diseases like influenza and tuberculosis.
The pulmonary route offers several advantages, including the ability to bypass the systemic circulation and deliver drugs directly to the target site, high bioavailability, and rapid onset of therapeutic effect.
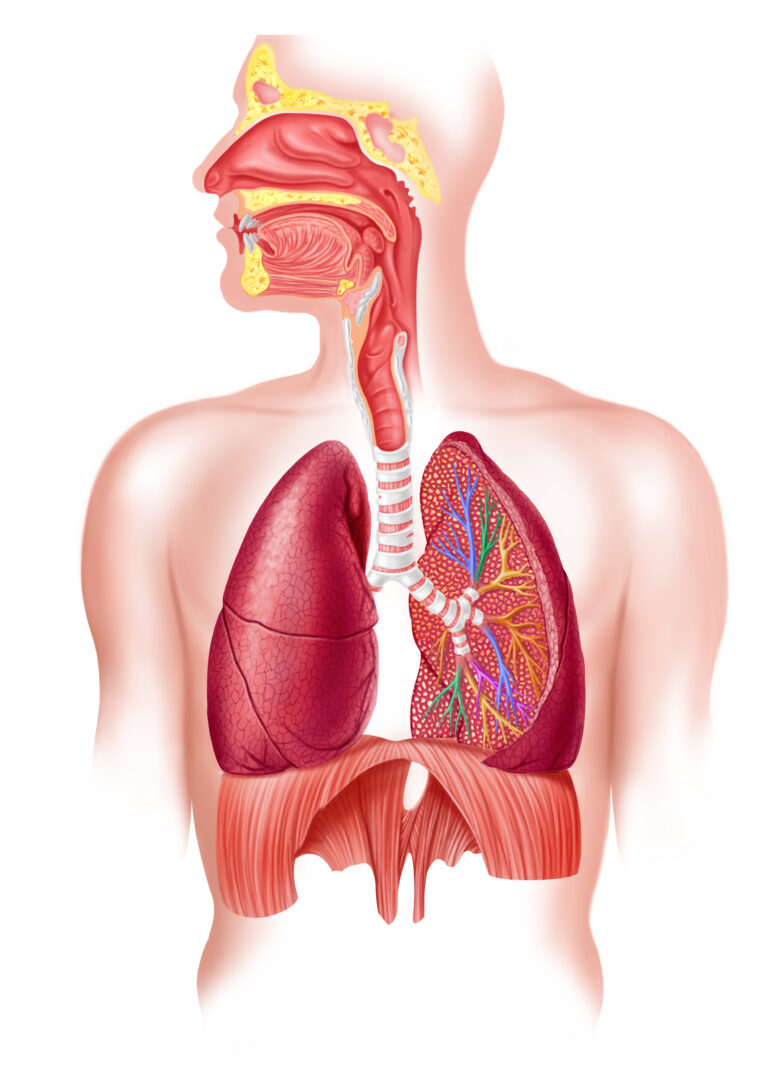
Optimal Site of Deposition for Treating Lung Diseases
Choosing the right site for drug deposition in the lungs is critical for treatment success. The primary target is the alveolar region, located deep in the lungs. This region has a large surface area for drug absorption due to its proximity to the pulmonary epithelium. The rich blood flow in alveoli ensures quick absorption and distribution throughout the body.
Targeting the alveolar region helps treat conditions like asthma, COPD, and cystic fibrosis more effectively. Depositing drugs in this area allows them to bypass mucociliary clearance, reaching the bloodstream faster and maximizing their therapeutic impact.
Factors Affecting Pulmonary Delivery
Several factors influence the effectiveness of pulmonary drug delivery. Particle size is crucial because it determines where the drug will deposit in the lungs. Smaller particles reach deeper areas, while larger particles tend to settle in the upper airways. Brownian motion also plays a role in particle distribution within the lungs.
Formulations must overcome mucociliary clearance to ensure prolonged residence and optimal absorption. The respiratory tract’s structure, including the surface area of the pulmonary epithelium, is another important consideration.
Other factors include the flow rate during inhalation, aerosol dispersion, and deposition mechanisms. These elements affect the performance of inhalers and delivery systems. Understanding these variables is essential for designing delivery systems that effectively target specific respiratory diseases. Advances in formulation design and delivery technology have addressed many of these challenges, leading to better patient compliance and treatment outcomes.

Advantages of Pulmonary Drug Delivery
Pulmonary drug delivery offers several advantages. The direct access to the pulmonary epithelium ensures faster drug absorption and a more potent therapeutic effect. In addition, the non-invasive delivery method reduces patient discomfort and improves adherence to treatment regimens.
Formulation design is crucial for maximizing delivery efficiency. Fine particles are preferred because they increase the surface area for absorption in the lungs. Dry powder inhalers (DPIs) have become popular due to their controlled delivery to the lungs, ensuring more efficient and targeted administration.
Overcoming Challenges
While pulmonary delivery offers many benefits, it comes with challenges. Drug solubility and stability are major factors affecting delivery system performance. Poor solubility can result in low bioavailability and reduced therapeutic efficacy. Formulation strategies, such as the use of solubility enhancers and nanoscale delivery systems, address these issues.
Drug stability is also critical. Factors like temperature, light exposure, and interactions between the drug and excipients can affect stability. Proper storage conditions and stability testing help maintain the drug’s effectiveness throughout its shelf life.
Regulatory considerations also play a role in implementing pulmonary delivery strategies. Compliance with guidelines for respiratory drug delivery systems is necessary for approval. Ethical considerations, such as ensuring patient safety and obtaining informed consent in clinical trials, must be addressed to maintain high standards in research and development.

Partnering with a CDMO for Pulmonary Drug Delivery
Partnering with a contract development and manufacturing organisation (CDMO) can streamline the development of pulmonary delivery systems. CDMOs offer expertise in formulation design, device selection, in vitro and in vivo testing, and regulatory compliance.
By working with a CDMO, healthcare professionals and pharmaceutical companies can accelerate the development and commercialization of delivery systems. CDMOs help navigate regulatory guidelines and address ethical considerations, ensuring safe and compliant solutions. This partnership allows for faster development cycles and more efficient delivery system implementation.
Collaborating on Formulation Development and Scale-Up
Successful pulmonary delivery relies on collaboration between healthcare professionals, pharmaceutical companies, and CDMOs. Formulation development focuses on optimizing factors like particle size, drug solubility, stability, and aerosol performance. Collaboration among these stakeholders enables the development of innovative and effective delivery systems.
Scale-up involves manufacturing the delivery system on a larger scale while maintaining consistency and quality. Working with a CDMO ensures that the manufacturing process adheres to strict standards, delivering reliable and effective products.
Criteria for Selecting the Right CDMO Partner
Selecting a suitable CDMO is critical for implementing effective pulmonary delivery strategies. Here are key criteria to consider:
- Expertise and Experience: Look for a CDMO with a proven track record in pulmonary delivery, including formulation design, device selection, and regulatory compliance.
- Infrastructure and Resources: Ensure the CDMO has the facilities and resources to support the development and manufacturing of respiratory delivery systems.
- Regulatory Compliance: The CDMO should understand international regulatory requirements and comply with relevant guidelines.
- Collaboration and Communication: A collaborative approach and clear communication between healthcare professionals and CDMOs are crucial for a successful partnership.
The Future of Pulmonary Drug Delivery
The future of pulmonary drug delivery in the UK, Europe, and North America looks promising. Advances in technology and a focus on personalized medicine will drive innovation. Smart inhalers, biologics, and digital health solutions are expected to improve treatment outcomes and patient adherence.
Collaborations between pharmaceutical companies, healthcare providers, and regulatory bodies will result in new delivery systems that focus on efficacy, safety, and patient convenience. The market is set to grow as research addresses unmet medical needs, improving outcomes for individuals with respiratory conditions.
Compliance with regulatory guidelines remains a priority, with CDMOs playing a crucial role in bringing these innovations to market. The goal is to provide more effective and tailored treatments, enhancing the quality of life for patients globally.
Healthcare professionals and pharmaceutical companies can select the right CDMO partner to streamline the development process and ensure the successful implementation of pulmonary delivery strategies.
Emerging Trends in Pulmonary Drug Delivery
Several trends are shaping the future of pulmonary drug delivery in the UK, Europe, and North America. There is a strong emphasis on personalized medicine and advanced technologies. Research is focused on developing delivery systems tailored to individual patient needs, improving outcomes through targeted therapies.
Strategic partnerships between healthcare professionals and pharmaceutical companies are key to advancing these technologies. Regulatory compliance remains a significant consideration, with CDMOs ensuring that new solutions meet international standards.
Nanotechnology is emerging as a vital tool for targeting specific areas of the lungs, maximizing therapeutic effects while minimizing side effects. Inhalable biologics are also gaining attention, offering new treatments for respiratory conditions like asthma and COPD.
Digital health technologies are integrating into delivery systems, enabling real-time monitoring of patient adherence and treatment responses. This allows for personalized treatment adjustments, ensuring better patient compliance and treatment outcomes.
Conclusion
Implementing pulmonary delivery strategies requires careful attention to formulation design, device selection, and regulatory compliance. Addressing challenges related to drug solubility, stability, and regulatory requirements is essential. Partnering with a CDMO can streamline development, ensuring successful formulation development and scale-up.
Collaborating with experts in the field enables healthcare professionals and pharmaceutical companies to navigate the complexities of pulmonary drug delivery more efficiently. This approach offers significant advantages over traditional administration routes, making it a valuable strategy for pharmaceutical advancements. As technology and research continue to evolve, pulmonary delivery systems will improve, offering more effective treatments and better patient outcomes.
Let's work together
How can we help you?
Frequently Asked Questions
How can small to medium-sized companies get started with pulmonary drug delivery?
Partnering with a contract development and manufacturing organization (CDMO) can streamline the development process by leveraging the CDMO’s expertise and resources. The CDMO can provide specialized capabilities in formulation design, device selection, in vitro and in vivo evaluation, and regulatory compliance, leading to greater efficiency and collaboration in the development of pulmonary delivery strategies.
How can partnering with a CDMO streamline the development process?
Small to medium-sized companies can get started with respiratory delivery by collaborating with contract development and manufacturing organizations (CDMOs) that have expertise and resources in pulmonary delivery. The CDMO can provide guidance and support in formulation design, device selection, and regulatory compliance, helping small to medium-sized companies navigate the complexities of pulmonary drug delivery.
What factors should be considered when designing a pulmonary drug delivery system?
Pulmonary delivery offers several advantages over other routes of administration. It allows drugs to be delivered directly to the lungs, bypassing the systemic circulation and maximizing the therapeutic effect. The large surface area of the lungs and the thin alveolar epithelial cell membrane facilitates rapid absorption and high bioavailability of drugs.
What are the advantages of pulmonary delivery over other routes of administration?
Implementing pulmonary delivery strategies can be challenging due to factors such as drug solubility and stability, regulatory considerations, and ethical considerations. It is important to address these challenges and limitations to ensure the successful implementation of respiratory delivery strategies.
Are there any challenges or limitations associated with implementing pulmonary drug delivery strategies?
When designing a pulmonary delivery system, several factors should be considered. These include the specific drug and patient needs, the target site of drug action in the lungs, particle size and deposition, and the choice of delivery device. By considering these factors, healthcare professionals can design an efficient and effective pulmonary delivery system.
Get in touch.
If you’re looking to work with a CDMO that can support your product from preclinical development to market and beyond, then we’re here to help.